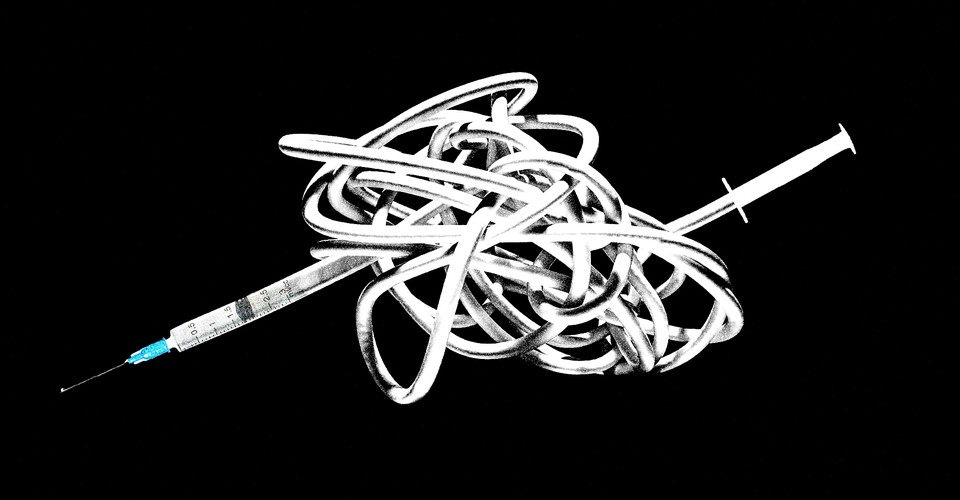
On the day that a COVID-19 vaccine is approved, a vast logistics operation will need to awaken. Millions of doses must travel hundreds of miles from manufacturers to hospitals, doctor’s offices, and pharmacies, which in turn must store, track, and eventually get the vaccines to people all across the country. The Centers for Disease Control and Prevention, along with state and local health departments, coordinates this process. These agencies distributed flu vaccines during the 2009 H1N1 pandemic this way, and they manage childhood vaccines every day. But the COVID-19 vaccine will be a whole new challenge.
“The COVID situation is significantly different and more complex than anything that we have had to deal with in the past,” says Kris Ehresmann, an infectious-disease director at the Minnesota Department of Health.
The two leading vaccine candidates in the U.S.—one developed by Moderna, the other by a collaboration between Pfizer and the German company BioNTech—have progressed so quickly to clinical trials precisely because they are the fastest to make and manufacture. They rely on a novel vaccine technology whose advantage is speed, but whose downside is extreme physical fragility. These vaccines have to be frozen—in Pfizer/BioNTech’s case, at an ultracold –94 degrees Fahrenheit, colder than most freezers—which will limit how and where they can be shipped. The ways these vaccines are formulated (without added preservatives) and packaged (in vials that hold doses for multiple people) also make them easier to develop and manufacture quickly but harder to administer on the ground.



Recent Comments